Fluids flow on application of pressure. The flow may be laminar flow that is orderly in parallel layers or turbulent flow that is chaotic. During laminar flow the layer closest to the wall is the slowest and the layer farthest, fastest. Viscosity, the internal friction between these layers, is a measure of thickness of a fluid. The higher the viscosity, thicker the fluid. Depending on whether the viscosity of fluids changes with flow rate or not fluids may be Newtonian of non-Newtonian. The viscosity of Newtonian fluids like water, honey and oil does not change with flow rates. The viscosity of blood, a non-Newtonian fluid, Blood viscosity increases with falling shear rates. The increase is dramatic at low shear rates. Blood viscosity depends on plasma viscosity and the type and number if blood cells.
Determinants of plasma viscosity
Plasma viscosity varies with the concentration of its constituents. Fibrous proteins like fibrinogen contribute more to plasma viscosity than globular proteins like albumin. Acute phase reactants increase plasma viscosity. Of the plasma constituents immunoglobulins and cholesterol are clinically relevant. Clinically significant increases in viscosity are most common in patients with increased immunoglobulin, both monoclonal and polyclonal. The commonest cause of hyperviscosity syndrome is increased IgM in patients with of Waldenström’s macroglobulinaemia. Patients with IgG3 and IgA multiple myeloma, cryoglobulinemia, both monoclonal and polyclonal and patients with polyclonal gammopathies may have hyperviscosity. Very high cholesterol levels in patients with primary biliary cirrhosis have also been associated with hyperviscosity. Plasma viscosity decreases with temperature.
Effect of Number and Type of Cells on Viscosity
Haematocrit and cell deformity affect blood viscosity. Blood viscosity increases with haematocrit in an exponential manner. There is a pronounced increase in viscosity at haematocrits more than 55%.
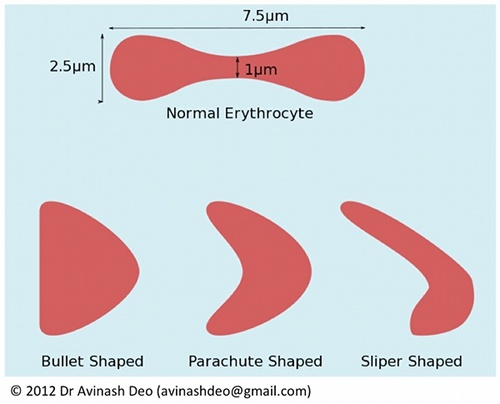
Blood cells disrupt flow lines of plasma and increase viscosity. Erythrocytes are the most numerous and under physiological conditions the flow properties of blood depend on the properties of plasma and erythrocytes. The normal erythrocyte is a biconcave disk about 7.8 µm in diameter (figure 1). At low flow rates erythrocytes aggregate in the form of stacks known as rouleaux. These large aggregates cause a sharp increase in viscosity. With increasing flow rates the shear stress on the erythrocyte rouleaux increases causing the erythrocytes to disaggregate. Disaggregation reduces viscosity. Any reduction in viscosity after complete disruption of rouleaux depends on the capacity of the erythrocyte to change so that resistance offered to flow decreases. The erythrocyte may take a bullet, parachute or a slipper form (figure 1). The deformability needed for shape change depends on the amount of surplus membrane, the properties of membrane and the viscous properties of the erythrocyte cytoplasm. RBC deformability is decreased in patients with hereditary spherocytosis because of decreased amount of membrane and in sickle cell anaemia because altered viscosity of haemoglobin and membrane damage. Malaria is characterized by deceased deformability and increased adhesiveness. Increased viscosity is responsible clinical manifestations of sickle cell anaemia and malaria. Intracellular crystallization of haemoglobin causes increased viscosity in haemoglobin C disease.
Figure 1. Deformability and aggregation of erythrocytes is responsible for changes in viscosity of blood as the flow rate increases. The normally biconcave erythrocyte aggregate into rouleaux at low flow rates. As the shear stress increases because of increased flow, the rouleaux disaggregate. Further increase in viscosity results in change in shape of the erythrocyte from biconcave to bullet shaped, parachute shapes and slipper shaped forms. These shapes offer less resistance to floe than the biconcave forms. Erythrocytes have about 40% surplus membrane. This surplus is important for shape change. Erythrocyes with viscous cytoplasm (HbS and HbC) resist change in shape increasing viscosity of blood in these diseases.
Leukocytes are larger than erythrocytes. As opposed to an erythrocyte volume of 80-90 (femtoliter) fL, the volume of a leukemic lymphocyte is 190-250 fL, lymphoblast is 250-350 fL and myeloblast is 350-450 fL. Viscosity depends on haematocrit. The contribution of leucocytes to normal haematocrit is small (~1.2%). Under physiological conditions haematocrit is practically equal to erythrocrit. Leucocytes are larger and less deformable because of the presence of a rigid nucleus. For a similar increase in count the leukocrit rises more than erythrocrit. Acute leukaemia is characterized by progressively increasing anaemia as the leukocyte counts increase. As the increased leukocrit is more than offset by anaemia in almost all patients with acute leukaemia, hyperviscosity is rare in acute leukaemias. There is an inverse relationship between leukocrit and erythrocrit in leukaemias for leukocrit values less than 15% for chronic leukaemias. The lymphocytes of chronic lymphocytic leukaemia are small and counts needed for a pathological increase haematocrit are rarely reached. Anaemia in patients of chronic myeloid leukaemia is less severe than acute leukaemia. Myeloid cells are larger than lymphoid cells. This makes patients with CML at the greatest risk for hyperviscosity. Anaemia is leukaemia protects from hyperviscosity. This must be borne in mind before initiating red cell transfusions in leukaemia patients.
Reading
- Blood rheology and hemodynamics. Baskurt OK, Meiselman HJ. Semin Thromb Hemost. 2003 Oct;29(5):435-50.
- Oguz K. Baskurt. Max R. Hardeman. Michael W. Rampling and Herbert J. Meiselman. Handbook of Hemorheology and Hemodynamics. 2007. IOS press. ISBN 978-1-58603-771-0 [Preview at Google Books